Chronic obstructive pulmonary disease
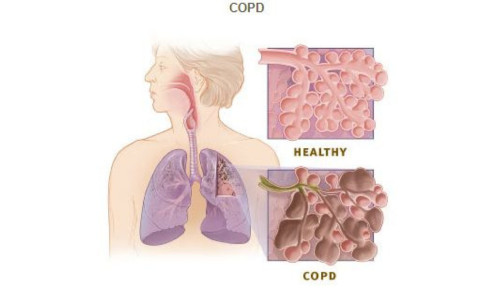
COPD is a chronic inflammatory lung disease that commonly affects both men and women worldwide. In patients with COPD, the airways may narrow due to a number of factors and processes, including abnormalities in the airways. There are two types of COPD — emphysema and chronic bronchitis. Emphysema affects the lungs’ alveoli (air sacs) and the walls between them; the air sacs get damaged and lose their elasticity. In chronic bronchitis, the lining of the airways is constantly inflamed — which causes it to swell and produce excess mucus.
Let’s take a look at some of the factors that can cause COPD:
- Smoking (Major cause)
- Exposure to certain dust and chemicals
- Exposure to fumes from burning fuels
- Genetics (individuals with alpha-1-antitrypsin deficiency are more at risk of developing COPD)
What are the common symptoms and signs of COPD?
In the early stage, patients may be asymptomatic (no symptoms) or present with mild symptoms. However, with the progression of the disease, the symptoms become severe. Some of the common symptoms include:
- Persistent cough with phlegm
- Frequent lung infections
- Shortness of breath
- Wheezing
- Chest tightness
- Fatigue
What to expect when you see a pulmonologist for COPD: Diagnosis and treatment of COPD
There are several tools that may be used to diagnose the condition:
- Detailed medical and family history
- Investigations such as spirometry (breathing test), blood investigations and imaging.
Based on the results of these investigations, the doctor will diagnose the condition and start the appropriate COPD treatment.
COPD is typically managed according to the Global Initiative for Obstructive Lung Disease (GOLD) guidelines. The GOLD guidelines are used to classify COPD severity and provide recommendations for first-line treatment. Medications such as bronchodilators, oral steroids, inhaled steroids, combination inhalers, and antibiotics may be prescribed. The doctor may advise on steps such as smoking cessation and vaccination. Treatment may vary depending on the patient, symptoms, stage (early or advanced), severity, and compliance.
COPD exacerbation
If a patient progresses rapidly from a stable condition to a severe one, it is referred to as a COPD exacerbation or flare-up. Exacerbations can last for days or even weeks. The two most common triggers for an exacerbation are respiratory tract infections, such as pneumonia and air pollution. There are some warning signs that may indicate a flare-up: more coughing, changes in the mucus (colour, thickness, and amount), and breathing difficulties.
Patients must seek immediate medical attention if the following occurs:
- Severe shortness of breath
- Chest pain
- Bluish discolouration of lips or fingers
- Confusion or difficulty in speaking a complete sentence
What happens at the clinic?
Patients may be referred to a pulmonologist for a severe and persistent cough lasting more than three weeks and/or any of the following symptoms:
- Chest tightness or pain
- Wheezing
- Fatigue
- Breathing difficulties
- Dizziness or lightheadedness
The pulmonologist will take a detailed medical history and physical examination at the first visit and may order investigations to diagnose and manage the condition. The patient should bring any records of blood work and imaging to be assessed by the pulmonologist. In addition, it is wise to be prepared with any questions or doubts so that these can be clarified at the clinic.